Respiratory Team
On this page
- Download the leaflet
- Introduction
- What causes this condition?
- Signs and symptoms
- How is Empyema diagnosed?
- What treatments are available?
- How long will my child be in hospital?
- Does anything increase the risk of acquiring an Empyema?
- What are the implications for others (risk of infection to other people)
- How long will my child need to stay off school or nursery?
- Will my child suffer from recurrent chest problems in the future?
- Who do I contact if worried once my child is discharged home?
Download the leaflet
Introduction
This leaflet is aimed at providing parents and carers with information about Empyema.
What causes this condition?
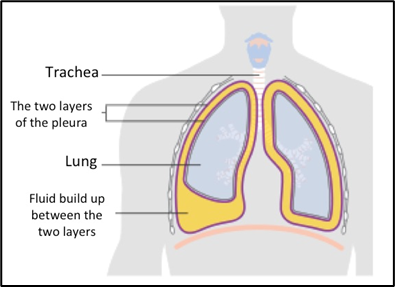
Empyema is a condition where pus builds up in the pleural space in your child’s chest, often as a complication of a chest infection (pneumonia).
The lungs and inside of the chest cavity have a smooth covering called the pleura that lets the lungs expand without rubbing on the inside of the chest. The two layers of pleura are usually in close contact with only a small space in between (pleural space) filled with a small amount of pleural fluid acting as lubrication.
This complication of pneumonia usually occurs in three stages. Initially, clear fluid builds up in the pleural space which can then become infected. The fluid thickens and can affect the pleura, causing sections to ‘stick together’ eventually forming ’pockets’– this is called empyema. The infected fluid stops the lungs inflating completely, causing breathing difficulties.
Signs and symptoms
Empyema is usually suspected when a severe case of pneumonia is not improving with antibiotic treatment. Children usually show symptoms of being generally unwell with a high temperature and often a cough. They may find their breathing is harder than normal and struggle to catch their breath. Their heart rate may also be higher than usual. Some children may describe pain in their chest when breathing.
How is Empyema diagnosed?
If empyema is suspected, a chest x-ray may be the first test suggested to confirm or rule out the diagnosis. Parts of the lung that are collapsed down due to the pneumonia, or where fluid is filling the space will appear white on the chest x-ray. An ultrasound of the chest can then be used to differentiate between collapsed lung and fluid. The ultrasound can also estimate how much fluid is present and where.
If a collection of fluid is located and requires draining, a sample will be tested in the laboratory to try and identify the bacteria causing the infection. This helps the team prescribe the most effective medication to treat it correctly. We will also take a sample of blood for the same reason. Other blood tests will help to monitor the infection and recovery.
What treatments are available?
If a small amount of fluid is identified on ultrasound, your child might be managed conservatively with antibiotics through their vein, also known as intravenously (IV), along with close observation. If there is a lot of infected fluid in the pleural space, this will need to be drained by inserting a chest drain. Most children have chest drains inserted when they are put to sleep (under a general anesthetic). If your child needs a chest drain they will also need IV antibiotics as well as a medication inserted into the chest drain to loosen the thick areas of pus, making it easier to drain. Oxygen and extra fluids (either orally or IV) may also be needed. They will have regular pain relief as the drain can be uncomfortable.
Some children will require more invasive surgery known as videoâ€assisted thoracoscopic surgery. The decision whether to insert a drain of perform surgery will be made jointly by the Respiratory and Surgical Teams in discussion with you.
In addition, your child will go home with a 2 week course of oral antibiotics to complete the treatment course.
How long will my child be in hospital?
It is very hard to predict your child’s length of stay, on average this may be around
2 weeks however this can be longer depending on their recovery.
Does anything increase the risk of acquiring an Empyema?
There are no clear predisposing factors for developing an Empyema other than contracting a severe pneumonia. In most cases, this complication is an unlucky consequence of the pneumonia and does not suggest your child has an underlying lung problem.
What are the implications for others (risk of infection to other people)
Most pneumonia that leads to empyema are community acquired, transmitted by an infected individual coughing or sneezing. There is a chance that people near to your child may contract the pneumonia, but no suggestion that they will develop an empyema.
How long will my child need to stay off school or nursery?
Most children fully recover and can return to school within a week of discharge from hospital, with gradual introduction of sports when they feel well enough. Each child is individual and will vary with their recovery time.
Will my child suffer from recurrent chest problems in the future?
There is no evidence to suggest your child will suffer with further chest complications and usually make a full recovery. The Respiratory team will follow your child up in clinic for a period of time to ensure there are no lasting complications.
Who do I contact if worried once my child is discharged home?
If within 1-2 weeks of discharge your child develops a fever or increased work of breathing, please seek medical review in your local area.
If you have any other non-urgent concerns, please contact the Respiratory Pathway
Co-ordinators for advice from the Respiratory Team on 0151 252 5777 or email: [email protected]
This leaflet only gives general information. You must always discuss the individual treatment of your child with the appropriate member of staff. Do not rely on this leaflet alone for information about your child’s treatment.
This information can be made available in other languages and formats if requested.
PIAG 353