Vascular Access Team
Information for parents and carers
On this page
- Download the leaflet
- What is a Broviac/Hickman line?
- Why does my child need a Broviac/Hickman line?
- What does a Broviac/Hickman line look like?
- Do I have to give my permission for it to be put in?
- How will my child be prepared?
- How long will it take to put in?
- Will it hurt?
- Are there any complications?
- What will happen if I do not have a bronchoscopy?
- Side effects
- How long will the bronchoscopy take?
- What are the benefits?
- Is there any other treatment my child could have?
- Can my child go home with a central line?
- What support will I get at home?
- What should I be looking for?
- What should I do if something goes wrong?
- Can my child still have a bath/shower?
- Can my child still play sports?
- Aseptic Non-Touch Technique (ANTT)
Download the leaflet
My child needs a Broviac/Hickman Line (257kB pdf)
What is a Broviac/Hickman line?
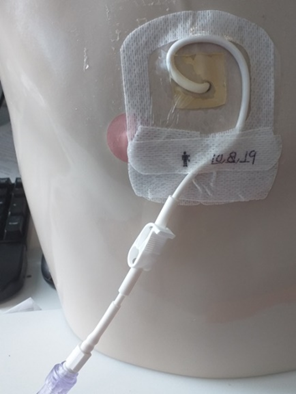
You may also hear it called a central line. It is a long thin rubber tube inserted into your child’s chest. The end of the tube sits in a large blood vessel near to or in part of their heart. The other end of the tube is white, and this is what you will see coming out of the skin at the exit site.
Why does my child need a Broviac/Hickman line?
A central line is needed when it is expected that the treatment your child requires through their veins (intravenously) could continue for quite a long time. This could include blood tests / products, intravenous feeding, medications or fluids.
What does a Broviac/Hickman line look like?
Do I have to give my permission for it to be put in?
Yes, inserting the line does mean your child having a small operation and a general anaesthetic for which your consent is required. Any risks to your child will be discussed with you by your child’s surgeon.
How will my child be prepared?
The ward staff will help to prepare your child and may use an information booklet to help them which is written for children.
How long will it take to put in?
This can vary from child to child and the surgeon will discuss this with you when you consent to treatment.
Will it hurt?
The procedure won’t hurt as your child is under general anaesthetic. Pain relief can be given when they wake up if the insertion site feels a little sore.
Are there any complications?
Bronchoscopy is usually a safe and straightforward procedure.
What will happen if I do not have a bronchoscopy?
Any side effects or complications will be discussed with you by your child’s anaesthetist and surgeon , but possible complications can be:
- Blockage. We try to prevent this by following a regular flushing routine of the line. This can try to be resolved by putting a special flush into the central line.
- Not bleeding back. This can be disappointing (because the central line can no longer be used to take blood), but it can still be used to give medications. We can try to resolve this by putting a special flush into the central line and we may need to check the position of the end of the central line. This is done by injecting dye into the line then performing a special x-ray.
- Leakage. This may occur if a forceful flush is attempted when the line is blocked. A special x-ray can see if the central line is working properly.
- Infection. Local infection can be treated with antibiotics, but occasionally, if the central line itself becomes infected, it may have to be removed.
- Loose clamp. This can come loose overtime due to continuous use. We may add an additional clamp onto the line. However, without the clamp in use, the needle-free devices (bungs) on the end of the line do provide positive pressure into the line to help prevent back flow of blood.
- Splitting. A fracture/break may occur in the line, if this occurs you must follow the emergency procedures you have been trained to do and immediately contact the community team or the contact provided by the ward staff on your discharge. You will be asked to bring your child into the hospital for a line assessment, or for a repair/ replacement line. If you are unable to contact anyone, please attend your nearest A&E department.
Side effects
These are the unwanted but mostly temporary effects of a successful procedure. Your child will feel sore and have some swelling and bruising around the entry and exit site
How long will the bronchoscopy take?
The bronchoscopy and lavage will take about 10 minutes. You will be asleep for about an hour while we do the bronchoscopy, lavage and insert a long line, if a long line is needed.
What are the benefits?
Having a central line may mean that your child will not need as many needles over the course of their treatment. Central lines can stay in place throughout your child’s treatment as long as there are no problems with the line. This may be months or years depending on the care your child needs.
Is there any other treatment my child could have?
Your child needs to have a central line put in because it is expected that they need to have blood tests, medication, fluids or special intravenous feeding. If a central line is not put in then your child could need a cannula and depending on your child’s treatment a cannula may not be a suitable line to be used and will mean more needles for your child, a central line will make treatment easier and more comfortable for your child.
Can my child go home with a central line?
Yes. You will be given information on caring for your child and their line at home eg/ bathing etc. There is also the option to be trained to access the line. If you do not wish to be trained to access the line care will done with the support of the Community Nursing Team.
You will be discharged home with an “emergency kit” this will include gauze, plastic blue clamps, and occlusive dressings. You will receive training on what to do in situations were the kit is required prior to being discharged home.
What support will I get at home?
The Community Nursing Team will support you at home.
What should I be looking for?
You should be looking at the site where the line comes through the skin and the surrounding area on your child’s chest to ensure that there is no redness, swelling, tracking (a red line along the skin) or is causing any pain.
You should also ensure that the clamp is always closed when not in use. The clamp should be clamped on the thicker part of the line and moved around to avoid wear in the same area.
What should I do if something goes wrong?
You can contact the Community Nursing Team, or the ward staff can give you information.
If you think your child is unwell and has a temperature, then you should take them straight to the nearest A&E department.
Can my child still have a bath/shower?
For the first four weeks following having the central line put in, the exit site should be kept dry. If the site is well healed and shows no sign of redness or oozing, then your child may have a shower. Do not use soap or shower gel directly around the site. If bathing then your child should sit in a shallow, waist deep bath. Do not allow your child to submerge or soak in the bath and keep the central line out of the water.
Can my child still play sports?
If your child has a central line in, they will be unable to go swimming and vigorous contact sports like rugby are not encouraged as your child’s central line may get pulled out accidentally.
Aseptic Non-Touch Technique (ANTT)
Your child’s central line will be accessed in order to deliver medication, blood products or fluids via a trained nurse or doctor. The technique used to access you child’s central line is called ANTT / Aseptic Non-Touch Technique. This is an evidence based clinical practice for preparation and administration of intravenous therapy. Research shows that using ANTT is best clinical practice for accessing intravenous lines and reducing risk of infection.
You should see:
- The nurse / doctor cleans their hands with soap and water or alcohol gel.
- Put on a pair of gloves prior to accessing your child’s line.
- Scrub the end of the intravenous line device for 20 seconds with a large wipe and allow it to dry for 20 seconds.
- Gather all equipment safely and remove it from your child’s bed space once the medication has been administered.
This leaflet only gives general information. You must always discuss the individual treatment of your child with the appropriate member of staff. Do not rely on this leaflet alone for information about your child’s treatment.
This information can be made available in other languages and formats if requested.
PIAG 22