Feeling sick and then vomiting is usually the first sign that your child has a ‘tummy bug’. Diarrhoea tends to occur after your child has started vomiting and means passing frequent watery poos that are offensive in nature.
- Tummy bugs are extremely common in young children and are almost always caused by a virus. They are easily spread, resulting in outbreaks in nurseries and schools
- Babies under 1 year of age (and especially under 6 months of age) are at more risk of becoming dehydrated when they have a tummy bug than older children, which is why it is important to make sure that they are drinking enough
Watch a video by one of Alder Hey’s doctors on gastroenteritis
Watch an Operation Ouch video on diarrhoea and vomiting that you can watch with your child
When should I worry and what should I do?
Call 999 or go to A&E now if your child:
Becomes pale, mottled and feels abnormally cold to touch
Going blue around the lips or too breathless to talk/eat or drink
Becomes extremely agitated, confused or very lethargic (difficult to wake)
Develops a rash that does not disappear with pressure (the ‘Glass Test’)
Call 111 or ask for an urgent GP appointment if your child:
Seems dehydrated or has not passed urine for 12 hours
Has blood in the stool (poo)
Has constant tummy pain
Has completely stopped drinking or breastfeeding
Is unable to keep down any fluids during this illness
Is becoming drowsy (excessively sleepy) or irritable (unable to settle them with cuddles, toys, TV, or snacks) – especially if they remain drowsy or irritable despite any fever coming down
Is 3 to 6 months of age with a temperature of 39°C / 102.2°F or above (but fever is common in babies up to 2 days after they receive vaccinations) (children under 3 months of age with a fever need to be seen in A&E)
If your child has diabetes, monitor their blood sugars closely.
If your child has a chronic condition affected by severe sickness, follow their rescue plan from your specialist team
If none of the above symptoms are present:
Your child does not seem to have any symptoms of serious illness or injury
You can get general advice on the NHS website or from your local pharmacy
Self Care
- Avoiding dehydration is important – give your baby/child extra fluids. Give your baby oral rehydration solution (ORS) or half-strength apple juice (apple juice mixed with the same amount of water) in between feeds or after each watery stool. Little and often tends to work best – in hospital, babies are given 1 or 2 teaspoons (5 to 10 mls) of fluid to drink every 5 to 10 minutes. You can try using a syringe to give fluids to your child. Mixing the contents of the ORS sachet in dilute squash (not “sugar-free” squash) instead of water may improve the taste
- Do not stop giving your baby milk. If you are breastfeeding, continue doing so
- Do not worry if your child is not interested in solid food. If they are hungry, offer them plain food such as biscuits, bread, pasta or rice. It is advisable not to give them fizzy drinks as this can make diarrhoea worse
- To avoid spreading the virus, wash your hands with soap and water after changing nappies. Keep toilets clean and don’t share towels
- They should not return to school or any other childcare facility until 48 hours after the last episode of diarrhoea and/or vomiting
How long will your child’s symptoms last?
Vomiting tends to last for 1 to 2 days, and diarrhoea tends to last for about 5 days but can last longer.
The charts below show how long diarrhoea and vomiting last in children when they have a tummy bug. The faces represent 10 children who have seen their GP with a tummy bug. Green faces are those children who have recovered within that time period.
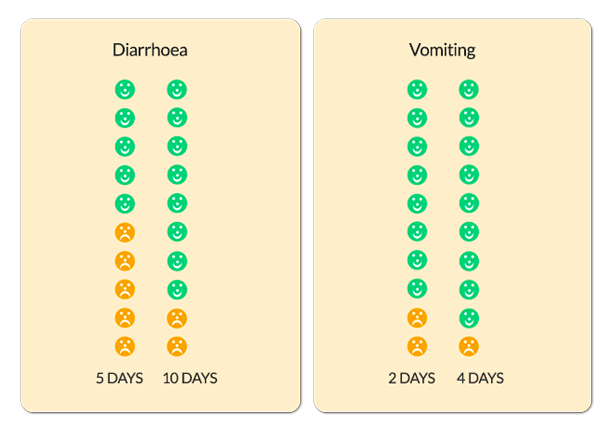
The diagram above is taken from When Should I Worry.
Where should you seek help?
- If it is non-urgent, speak to your local pharmacist or health visitor
- Or contact you GP practice and a qualified member of the clinical team will assess if your child needs to be seen urgently. For an urgent out-of-hours GP appointment, call NHS 111
- You should only call 999 or go your nearest A&E department in critical or life threatening situations