It is extremely scary if your child has any sort of breathing difficulty. Use your instincts; if your child appears well and their breathing difficulty improves after a short period, there is normally no need to worry.
Wheezing is extremely common in young children and is most often triggered by a viral infection. Most preschool children with wheezing do not have asthma.
Children under two years of age with breathing difficulty may have bronchiolitis. This is an extremely common condition that usually starts as a runny nose and cough, but their breathing may get worse over the next 2 to 3 days.
If your child is struggling to breathe, they need to be seen urgently by a medical practitioner and are likely to need treatment. If your child has croup (hoarse voice, barking cough, noisy breathing), they will also need to be seen by a medical practitioner.
Most chest infections are caused by viruses and do not usually need treatment with antibiotics.
Babies normally breathe at a faster rate than adults and older children. It is normal for a newborn baby to take slight pauses in their breathing for a few seconds, or to breathe rapidly for a short period. By 6 weeks of age, they should have a more regular breathing pattern.
Sometimes a baby’s breathing rate may increase for a longer period of time if they are unwell and you may also notice they are working harder to breathe. For babies, the most tiring thing they do is feeding, so this can be the first time you notice them struggling to breathe. If they are too breathless to feed, they need to be seen urgently by a healthcare professional.
It can be very scary watching your child having difficulty breathing and below are some signs to look out for if you are worried.
When should I worry and what should I do?
Call 999 or go to A&E now if your child:
Shows signs of working hard to breathe. These include constantly breathing fast, flaring of the nostrils, drawing in the muscles below the ribs or making a grunting noise every time they breathe out
Is going blue around the lips
Has long pauses in their breathing (more than 10 seconds) or has an irregular breathing pattern
A harsh breath noise as they breathe in (stridor) present all the time (even when they are not upset)
Too breathless to talk/feed or drink
Becomes pale, mottled and feels abnormally cold to touch
Becomes extremely agitated (crying inconsolably despite distraction), confused, floppy or very lethargic (difficult to wake)
Develops a rash that does not disappear with pressure (the ‘Glass test’)
Is under 3 months of age with a temperature of 38°C / 100.4°F or above (unless fever in the 48 hours following vaccinations and no other red or amber features)
Call 111 or ask for an urgent GP appointment if your child:
Has laboured/rapid breathing or they are working hard to breathe – drawing in the muscles below their lower ribs, at their neck or between their ribs (recession).
A harsh breath noise as they breathe in (stridor) present only when they are upset
Seems dehydrated (sunken eyes, drowsy or not passed urine for 12 hours)
Is becoming drowsy (excessively sleepy) or irritable (cuddles, toys, TV, or snacks) – especially if they remain drowsy or irritable despite their fever coming down
Has extreme shivering or complains of muscle pain
Is 3 to 6 months of age with a temperature of 39°C / 102.2°F or above (but fever is common in babies up to 2 days after they receive vaccinations)
Continues to have a fever of 38.0°C or above for more than 5 days
Is getting worse or if you are worried
If none of the above symptoms are present:
Make sure that your child stays well hydrated by offering them lots of fluids. And closely monitor them for any signs of deterioration by looking out for any symptoms listed above
If your child is interacting with you normally and can drink as normal, you can watch them closely at home. If your child is not feeding as well as normal, you should offer smaller feeds but more frequently
If they become more breathless or start or are struggling to drink, they will need to be seen urgently by a medical practitioner. Call your GP surgery or NHS 111
If your child has a fever, their breathing may become more rapid. You should try to lower their temperature using paracetamol (calpol)
You can get general advice on the NHS website or from your local Pharmacy
How long will your child’s symptoms last?
Although your child’s cough is likely to last for 2 to 3 weeks, they should not be breathless or wheezy for more than 3 or 4 days.
The charts below show how long croup or bronchiolitis lasts in children. The faces represent 10 children who have croup or bronchiolitis. Green faces are those children who have recovered within that time period.
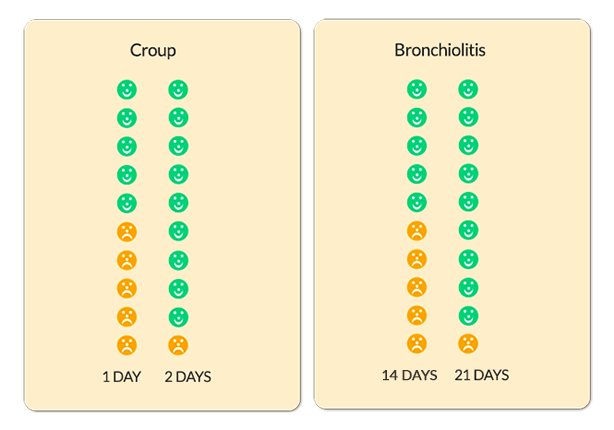
The diagrams above are taken from When Should I Worry.
Where should you seek help?
- If it is non-urgent, speak to your local pharmacist or health visitor.
- Or contact you GP practice and a qualified member of the clinical team will assess if your child needs to be seen urgently. For an urgent out-of-hours GP appointment, call NHS 111.
- You should only call 999 or go your nearest A&E department in critical or life threatening situations.